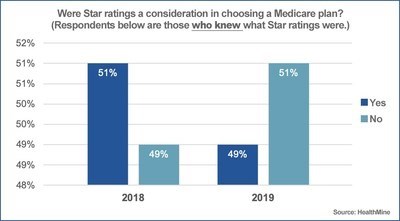
Only 32 percent of the 800 Medicare Advantage (MA) plan members with chronic conditions are familiar with the Centers for Medicare & Medicaid Services’ (CMS) star ratings systems, according to a HealthMine survey. Of those, nearly half said they used the grading system to help them choose a plan for 2019 enrollment.
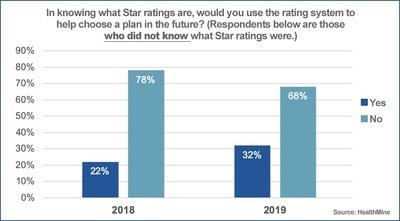
Once informed about the quality rating system, most (74 percent) of the remaining MA members who were unfamiliar with star ratings told HealthMine they would use them in the future to help them choose a plan.



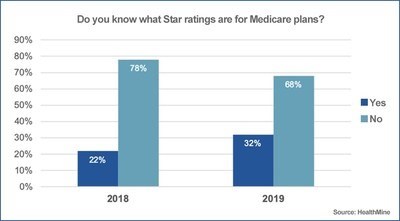
The survey responses show an improvement in awareness of the CMS star rating system. In 2018, only 22 percent of 781 MA plan members said they were familiar with the system.
"Awareness of star ratings is slightly on the rise, but still low at less than one in three people. Yet, most Medicare Advantage enrollees are ending up in the highest rated plans. We only expect that to grow and push to ubiquity where almost all members are in four-plus star rated plans,” said Jean Arrington, chief innovation officer at HealthMine.
This means health plans will face increased pressure to excel in a value-based insurance design world, according to Arrington. “The engine driving plan performance is clearly each member taking the right health actions. We are seeing that our health plan clients that create deep connections with members are realizing results with high star ratings,” she said.
Improving and maintaining quality of care measures are vital to the success of every health plan. Qualipalooza, the 4th Annual RISE Quality Leadership Summit, June 27-28, in Orlando, Fla. will feature nationwide, leading quality experts who will discuss best practices and strategies to improve star ratings as well as HEDIS® scores, CAHPS, and HOS. An entire track will be devoted to stars and includes presentations and panel discussions on how to improve performance by motivating the unengaged, how to enhance engagement strategies to bridge gaps in care, and strategies to achieve and maintain a 4-star-plus rating. For the complete agenda, click here.

